Attention deficit disorder - how to cope with a hyperactive child?
Capricious, restless children are a real punishment for parents and teachers. It is difficult for them not only to behave quietly in class, but also to simply sit quietly in one place. They are talkative, unrestrained, change their mood and type of activity almost every minute. It is almost impossible to capture the attention of a restless person, as well as to direct his violent energy in the right direction. Whether this is ordinary bad manners or a mental disorder, only a specialist can determine. What is the manifestation of attention deficit in children and how to treat this pathology? How can parents and teachers deal with this problem? We'll talk about everything related to ADHD below.
Signs of the disease
Attention deficit disorder is a behavioral disorder first described by a psychoneurologist from Germany back in the century before last. However, people started talking about the fact that this is a pathology associated with minor disorders of brain activity only in the mid-60s of the last century. Only in the mid-nineties did the disease take its place in the medical classification, and was called “Attention Deficit Disorder in Children.”
Pathology is considered by neurologists as a chronic condition, an effective treatment for which has not yet been found. An accurate diagnosis is made only in preschool age or when studying in the lower grades. To confirm it, it is necessary that the child prove himself not only in everyday life, but also in the learning process. Medical statistics show that hyperactivity occurs in 5-15% of schoolchildren.
Characteristic symptoms of child behavior with ADHD can be roughly divided into 3 categories.
- Inattention
The child is easily distracted from activities, forgetful, and unable to concentrate. It’s as if he doesn’t hear what his parents or teachers say. Such children constantly have problems completing tasks, following instructions, organizing free time and the educational process. They make too many mistakes, but not because they are not thinking well, but because of inattention or haste. They give the impression of being too absent-minded because they always lose something: personal belongings, toys, items of clothing.
- Hyperactivity
Children with this diagnosis are never calm. They constantly take off, run somewhere, climb poles and trees. In a sitting position, the limbs of such a child do not stop moving. He always swings his legs, moves objects on the table, or makes other unnecessary movements. Even at night, a baby or teenager too often turns around in bed, knocking down the bedding. In a group they give the impression of being overly sociable, talkative and fussy.
- Impulsiveness
They say about such children that their tongue gets ahead of their head. During a lesson, a child shouts out from his seat without even listening to the end of the question, and prevents others from answering, interrupting and getting forward. He does not know how to wait at all or delay getting what he wants for even a minute. Often such manifestations are considered by parents and teachers as character traits, although these are clear signs of the syndrome. 
Psychologists and neurologists note that the manifestations of pathology vary among representatives of different age categories.
- Kids are disobedient, overly capricious, and poorly controlled.
- Schoolchildren are forgetful, absent-minded, talkative and active.
- Teenagers tend to dramatize even minor events, constantly show anxiety, easily become depressed, and often behave demonstratively.
A child with such a diagnosis may show reluctance to communicate with peers and show rudeness towards peers and elders.
When does attention deficit disorder begin to appear in children?
Signs of pathology are indicated at an early age
Already in a 1-2 year old child, distinct symptoms of the disease are observed. But most parents accept this behavior as the norm or ordinary children's whims. No one goes to the doctor with such problems, missing out on important time. Children experience speech delay, excessive mobility with impaired coordination.
A three-year-old child is experiencing an age-related crisis associated with personal awareness. Whims and stubbornness are common accompaniments of such changes. But in a child with disabilities, such signs are more pronounced. He does not respond to comments and demonstrates hyperactivity; he simply does not sit still for a second. It is very difficult to put such a “live” to sleep. The formation of attention and memory in children with the syndrome noticeably lags behind their peers.
In children of primary preschool age, signs of ADHD include the inability to concentrate in class, listen to the teacher, or simply sit in one place. At the age of five or six years, children are already starting to prepare for school, the load, physical and psychological, increases. But since kids who have hyperactivity are slightly behind their peers in mastering new knowledge, they develop low self-esteem. Psychological stress leads to the development of phobias, and physiological reactions such as tics or bedwetting (enuresis) appear.
Students diagnosed with ADHD have poor academic performance, despite the fact that they are not stupid at all. Teenagers do not have good relationships with the staff and teachers. Teachers often classify such children as disadvantaged because they are harsh, rude, often conflict with classmates, and do not respond to comments or criticism. Among their peers, adolescents with ADHD also often remain outcasts because they are overly impulsive and prone to aggression and antisocial behavior.
Advice: Defiant behavior means that your child wants to attract attention, but does not yet know how to do it differently.
People started talking about attention deficit disorder as a neurological disease not too long ago in Russia and doctors still do not have enough experience in making a diagnosis. The pathology is sometimes confused with mental retardation, psychopathy, and even schizophrenic disorders. Diagnosis is also complicated by the fact that some of these signs are characteristic of ordinary children. Without careful analysis and long-term observation, it is difficult to determine why a child is inattentive during a lesson or is too active.
Causes of the disease
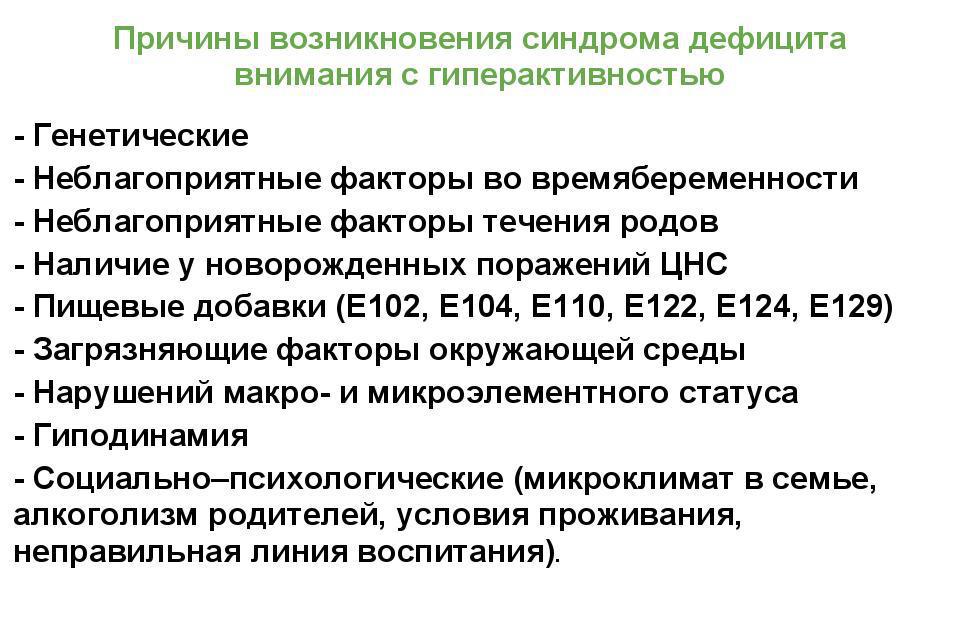
European and American doctors have been researching the syndrome for decades. Meanwhile, its reasons have not yet been reliably established. Among the main factors in the occurrence of pathology are usually called:
- genetic predisposition,
- birth injuries,
- nicotine and alcohol consumed by the expectant mother,
- unfavorable course of pregnancy,
- rapid or premature birth,
- stimulation of labor,
- head injuries at an early age,
- meningitis and other infections affecting the central nervous system.
The occurrence of the syndrome is facilitated by psychological problems in the family or neurological diseases. Pedagogical mistakes of parents and excessive strictness in upbringing can also leave some imprint. But the main cause of the disease is still considered to be a lack of the hormones norepinephrine and dopamine. The latter is considered a relative of serotonin. Dopamine levels increase during activities that a person finds enjoyable.
Interesting fact: since the human body is able to obtain dopamine and norepinephrine from certain foods, there are theories that the cause of ADHD in children is poor nutrition, for example, strict vegetarian diets.
It is customary to distinguish three types of disease.
- The syndrome can be represented by hyperactive behavior, but without signs of attention deficit.
- Attention deficit not associated with hyperactivity.
- Hyperactivity combined with attention deficit .
Correction of hyperactive behavior is carried out comprehensively and includes various techniques, including both medicinal and psychological. Europeans and Americans, when attention deficit is detected in children, use psychostimulants for treatment. Such drugs are effective, but have unpredictable consequences. Russian experts recommend mainly methods that do not include pharmacological agents. They begin to treat the syndrome with tablets if all other methods have failed. In this case, nootropic drugs are used that stimulate cerebral circulation or natural sedatives.
What should parents do if their child has attention deficit disorder?
- Physical activity. But sports games that include competitive elements are not suitable for them. They only contribute to excessive overstimulation.
- Static loads: wrestling or weightlifting are also contraindicated. Aerobic exercise, but in moderation, has a good effect on the nervous system. Skiing, swimming, cycling will allow you to use up excess energy. But parents need to make sure that the child does not become overtired. This will lead to decreased self-control.
- Working with a psychologist.
Psychological correction in the treatment of the syndrome is aimed at reducing anxiety and increasing the sociability of a child or teenager. To do this, techniques are used to modulate all kinds of success situations, thanks to which the specialist has the opportunity to observe the child and select the most suitable areas of activity for him. The psychologist uses exercises that promote the development of attention, memory, and speech. Communication with such children is not easy for parents. Often mothers who have a child with the syndrome themselves have signs of a depressive disorder. Therefore, families are recommended to work together with a specialist.
- Behavioral correction of attention deficit hyperactivity disorder in children involves positive changes in their environment. As the child achieves success in classes with a psychologist, it is better to change the environment of peers.
- With a new team, children find a common language easier, forgetting old problems and grievances. Parents also need to change their behavior. If excessive strictness has been practiced in upbringing before, you need to loosen control. Permissiveness and freedom must be replaced by a clear schedule. Parents need to compensate for the lack of positive emotions by praising their child more often for his efforts.
- When raising such children, it is better to minimize prohibitions and refusals. Of course, you shouldn’t cross the borders of reason, but only impose “taboo” on what is truly dangerous or harmful. A positive parenting model involves frequent use of verbal praise and other rewards. You need to praise your child or teenager even for small achievements.
- It is necessary to normalize relations between family members. You should not quarrel in front of your child.
Parents need to strive to gain the trust of their son or daughter, maintain mutual understanding, calm communication without shouting or commanding tone. - Joint leisure time for families raising hyperactive children is also very important. It would be good if the games were educational in nature.
- Children with similar problems need a clear daily routine and an organized place to study.
- Daily household chores that children carry out independently are very disciplined. Therefore, be sure to find several such tasks and monitor their implementation.
- Set adequate expectations for your child that match his abilities. There is no need to underestimate its capabilities or, on the contrary, overestimate them. Speak in a calm voice, turn to him with a request, not an order. Do not try to create greenhouse conditions. He must be able to cope with loads appropriate to his age.
- Such children need to devote more time than ordinary children. Parents will also have to adapt to the lifestyle of the younger family member, adhering to the daily routine. You shouldn’t forbid a child anything if it doesn’t apply to everyone else. It is better for babies and middle-aged children not to visit crowded places, as this contributes to overstimulation.
- Hyperactive children are capable of disrupting the educational process, but at the same time it is impossible to influence them in proven ways. Such children are indifferent to shouts, remarks and bad grades. But you still need to find a common language with an overly active schoolchild. How should a teacher behave if there is a child with ADHD in the class?
A few tips to help keep the situation under control:
- During the lesson, arrange short physical education breaks. This will benefit not only hyperactive, but also healthy children.
- Classrooms should be equipped functionally, but without distracting decor in the form of crafts, stands or paintings.
- To better control such a child, it is better to place him in the first or second desk.
- Keep active kids busy with errands. Ask them to wipe the board and hand out or collect notebooks.
- To better assimilate the material, present it in a playful way.
- A creative approach is effective in teaching all children without exception.
- Breaking tasks down into small chunks will make it easier for children with ADHD to navigate.
- Allow children with behavioral problems to express themselves in something necessary, to show their best side.
- Help such a student establish contact with classmates and take a place in the team.
- Exercises during the lesson can be done not only standing, but also sitting. Finger games are well suited for this purpose.
- Constant individual contact is required. It must be remembered that they respond better to praise; it is with the help of positive emotions that the necessary positive behavior patterns are reinforced.
Conclusion
Parents with a hyperactive child in their family should not brush aside the advice of doctors and psychologists. Even if the problem becomes less severe over time, the diagnosis of ADHD will have an impact in the future. In adulthood, it will cause poor memory and inability to control one’s own life. In addition, patients with a similar diagnosis are prone to various types of addictions and depression. Parents should become an example for their child, help him find a place in life, and gain faith in his own strength.
In every little child,
Both the boy and the girl,
There are two hundred grams of explosives
Or even half a kilo!
He must run and jump
Grab everything, kick your legs,
Otherwise it will explode:
Fuck-bang! And he’s gone!
Every new child
Gets out of diapers
And gets lost everywhere
And it is everywhere!
He's always rushing somewhere
He will be terribly upset
If anything in the world
What if it happens without him!
Song from the film “Monkeys, Go!”
There are children who were born to immediately jump out of the cradle and rush off. They cannot sit still for even five minutes, they scream the loudest and rip their pants more often than anyone else. They always forget their notebooks and write “homework” with new mistakes every day. They interrupt adults, they sit under desks, they don’t walk by the hand. These are children with ADHD. Inattentive, restless and impulsive,” these words can be read on the main page of the website of the interregional organization of parents of children with ADHD “Impulse”.
Raising a child with attention deficit hyperactivity disorder (ADHD) is not easy. Parents of such children hear almost every day: “I’ve been working for so many years, but I’ve never seen such disgrace,” “Yes, he has bad manners syndrome!”, “We need to hit him more!” The child has been completely spoiled!≫.
Unfortunately, even today, many specialists working with children know nothing about ADHD (or know only by hearsay and are therefore skeptical about this information). In fact, sometimes it is easier to refer to pedagogical neglect, bad manners and spoiling than to try to find an approach to a non-standard child.
There is also the other side of the coin: sometimes the word “hyperactivity” is understood as impressionability, normal curiosity and mobility, protest behavior, or a child’s reaction to a chronic traumatic situation. The issue of differential diagnosis is acute, because most childhood neurological diseases can be accompanied by impaired attention and disinhibition. However, the presence of these symptoms does not always indicate that a child has ADHD.
So what is attention deficit hyperactivity disorder? What is an ADHD child like? And how can you tell a healthy “butt” from a hyperactive child? Let's try to figure it out.
What is ADHD
Definition and Statistics
Attention-deficit/hyperactivity disorder (ADHD) is a developmental behavioral disorder that begins in childhood.
Symptoms include difficulty concentrating, hyperactivity, and poorly controlled impulsivity.
Synonyms: hyperdynamic syndrome, hyperkinetic disorder. Also in Russia, in the medical record, a neurologist can write for such a child: PEP CNS (perinatal damage to the central nervous system), MMD (minimal cerebral dysfunction), ICP (increased intracranial pressure).
First The description of the disease, characterized by motor disinhibition, attention deficit and impulsivity, appeared about 150 years ago, since then the terminology of the syndrome has been changed many times.
According to statistics, ADHD is more common in boys than in girls (almost 5 times). Some foreign studies indicate that this syndrome is more common among Europeans, fair-haired and blue-eyed children. American and Canadian experts use the DSM (Diagnostic and Statistical Manual of Mental Disorders) classification when diagnosing ADHD; in Europe, the International Classification of Diseases ICD (International Classification of Diseases) has been adopted ) with more stringent criteria. In Russia, diagnosis is based on the criteria of the tenth revision of the International Classification of Diseases (ICD-10), and also based on the DSM-IV classification (WHO, 1994, recommendations for practical use as criteria for the diagnosis of ADHD).
ADHD controversy
Disputes among scientists about what ADHD is, how to diagnose it, what kind of therapy to carry out - medicinal or using measures of a pedagogical and psychological nature - have been going on for decades. The very fact of the presence of this syndrome is also called into question: so far no one can say for sure to what extent ADHD is the result of brain dysfunction, and to what extent - the result of improper upbringing and the incorrect psychological climate prevailing in the family.
The so-called ADHD controversy has been going on since at least 1970. In the West (particularly in the USA), where drug treatment of ADHD is accepted with the help of potent drugs containing psychotropic substances (methylphenidate, dextroamphetamine), the public is alarmed that a large number of “difficult” children are diagnosed with ADHD and drugs containing drugs are unjustifiably often prescribed a lot of side effects. In Russia and most countries of the former CIS, another problem is more common - many teachers and parents are not aware that some children have characteristics that lead to impaired concentration and control. Lack of tolerance for the individual characteristics of children with ADHD leads to the fact that all the child’s problems are attributed to lack of upbringing, pedagogical neglect and parental laziness. The need to regularly make excuses for the actions of your child ("yes, we explain to him all the time" - "that means you explain poorly, since he does not understand") often leads to the fact that mothers and fathers experience helplessness and a sense of guilt, beginning to consider themselves worthless parents.
Sometimes it happens the other way around - motor disinhibition and talkativeness, impulsiveness and inability to comply with discipline and group rules are considered by adults (usually parents) to be a sign of the child’s outstanding abilities, and sometimes they are even encouraged in every possible way. ≪We have a wonderful child! He is not hyperactive at all, but simply lively and active. He’s not interested in these classes of yours, so he’s rebelling! At home, when he gets carried away, he can do the same thing for a long time. And having a quick temper is a character, what can you do about it,” some parents say, not without pride. On the one hand, these mothers and fathers are not so wrong - a child with ADHD, carried away by an interesting activity (assembling puzzles, role-playing games, watching an interesting cartoon - to each his own), can really do this for a long time. However, you should know that with ADHD, voluntary attention is primarily affected - this is a more complex function that is unique to humans and is formed during the learning process. Most seven-year-olds understand that during a lesson they need to sit quietly and listen to the teacher (even if they are not very interested). A child with ADHD understands all this too, but, unable to control himself, can get up and walk around the classroom, pull a neighbor’s pigtail, or interrupt the teacher.
It is important to know that ADHD children are not “spoiled,” “ill-mannered,” or “pedagogically neglected” (although such children, of course, also exist). This is worth remembering for those teachers and parents who recommend treating such children with vitamin P (or simply a belt). ADHD children disrupt classes, act out during breaks, are insolent and disobey adults, even if they know how to behave, due to objective personality traits inherent in ADHD. This needs to be understood by those adults who object to “diagnosing a child,” arguing that these children “just have that kind of character.”
How ADHD manifests itself
Main manifestations of ADHD
G.R. Lomakina in her book “Hyperactive Child.” How to find a common language with a restless person≫ describes the main symptoms of ADHD: hyperactivity, impaired attention, impulsivity.
HYPERACTIVITY manifests itself in excessive and, most importantly, confused motor activity, restlessness, fussiness, and numerous movements that the child often does not notice. As a rule, such children speak a lot and often confusedly, without finishing sentences and jumping from thought to thought. Lack of sleep often aggravates the manifestations of hyperactivity - the child’s already vulnerable nervous system, without having time to rest, cannot cope with the flow of information coming from the outside world and defends itself in a very peculiar way. In addition, such children often have problems with praxis—the ability to coordinate and control their actions.
ATTENTION DISORDERS manifest themselves in the fact that it is difficult for the child to concentrate on the same thing for a long time. His ability to selectively concentrate attention is not sufficiently developed - he cannot distinguish the main thing from the secondary. A child with ADHD constantly “jumps” from one thing to another: “loses” lines in the text, solves all examples at the same time, drawing the tail of a rooster, paints all the feathers at once and all colors at once. Such children are forgetful, do not know how to listen and concentrate. Instinctively, they try to avoid tasks that require prolonged mental effort (it is typical for any person to subconsciously shy away from activities, the failure of which he foresees in advance). However, the above does not mean that children with ADHD are unable to maintain attention on anything. They cannot focus only on what is not interesting to them. If they are fascinated by something, they can do it for hours. The trouble is that our lives are full of activities that we still have to do, despite the fact that they are not always exciting.
IMPULSIVITY is expressed in the fact that the child’s action often precedes thought. Before the teacher has time to ask the question, the ADHD student is already raising his hand, the task has not yet been fully formulated, and he is already completing it, and then, without permission, he gets up and runs to the window - simply because he became interested in watching how the wind blows from birch trees last leaves. Such children do not know how to regulate their actions, obey rules, or wait. Their mood changes faster than the direction of the wind in autumn.
It is known that no two people are exactly alike, so the symptoms of ADHD manifest differently in different children. Sometimes the main complaint of parents and teachers will be impulsivity and hyperactivity; in another child, attention deficit is most pronounced. Depending on the severity of symptoms, ADHD is divided into three main types: mixed, with severe attention deficit, or with a predominance of hyperactivity and impulsivity. At the same time, G.R. Lomakina notes that each of the above criteria can be expressed at different times and to varying degrees in the same child: “That is, to put it in Russian, the same child today can be absent-minded and inattentive, tomorrow - resemble an electric broom with with an Energizer battery, the day after tomorrow - move from laughing to crying and vice versa all day, and after a couple of days - fit inattention, mood swings, and irrepressible and confused energy into one day.
Additional symptoms common in children with ADHD
Coordination problems detected in approximately half of ADHD cases. These may include problems with fine movements (tying shoelaces, using scissors, coloring, writing), balance (children have difficulty riding a skateboard and two-wheeled bicycle), or visual-spatial coordination (inability to play sports, especially with a ball).
Emotional disturbances often observed in ADHD. The emotional development of a child, as a rule, is delayed, which is manifested by imbalance, hot temper, and intolerance to failures. Sometimes they say that the emotional-volitional sphere of a child with ADHD is in a ratio of 0.3 with his biological age (for example, a 12-year-old child behaves like an eight-year-old).
Disorders of social relations. A child with ADHD often experiences difficulties in relationships not only with peers, but also with adults. The behavior of such children is often characterized by impulsiveness, intrusiveness, excessiveness, disorganization, aggressiveness, impressionability and emotionality. Thus, a child with ADHD is often a disruptor to the smooth flow of social relationships, interaction and cooperation.
Partial developmental delays, including school skills, are known to be the discrepancy between actual academic performance and what would be expected based on a child's IQ. In particular, difficulties with reading, writing, and counting (dyslexia, dysgraphia, dyscalculia) are common. Many children with ADHD in preschool age have specific difficulties understanding certain sounds or words and/or difficulty expressing themselves in words.
Myths about ADHD
ADHD is not a perceptual disorder! Children with ADHD hear, see, and perceive reality just like everyone else. This distinguishes ADHD from autism, in which motor disinhibition is also common. However, in autism, these phenomena are caused by impaired perception of information. Therefore, the same child cannot be diagnosed with ADHD and autism at the same time. One excludes the other.
ADHD is based on a violation of the ability to perform a given task, an inability to plan, carry out, and complete a task begun. Children with ADHD feel, understand, and perceive the world in the same way as everyone else, but they react to it differently.
ADHD is not a disorder of understanding and processing received information! A child with ADHD is, in most cases, able to analyze and draw the same conclusions as anyone else. These children know very well, understand and can even easily repeat all those rules that they are constantly reminded, day after day: “don’t run”, “sit still”, “don’t turn around”, “keep quiet during the lesson”, “drive” behave just like everyone else,” “clean up your toys.” However, children with ADHD cannot follow these rules.
It is worth remembering that ADHD is a syndrome, that is, a stable, single combination of certain symptoms. From this we can conclude that at the root of ADHD lies one unique feature that always forms slightly different, but essentially similar behavior. Broadly speaking, ADHD is a disorder of motor function and planning and control, rather than perceptual and comprehension function.
Portrait of a hyperactive child
At what age can ADHD be suspected?
“Hurricane”, “tough in the butt”, “perpetual motion machine” - what definitions do parents of children with ADHD give their children! When teachers and educators talk about such a child, the main thing in their description will be the adverb “too”. The author of a book about hyperactive children, G.R. Lomakina, notes with humor that “there are too many such children everywhere and always, he is too active, he can be heard too well and far away, he is too often seen absolutely everywhere. For some reason, such children not only always end up in some kind of story, but such children also always end up in all the stories that happen within ten blocks of the school.”
Although today there is no clear understanding of when and at what age we can say with confidence that a child has ADHD, most experts agree that that this diagnosis cannot be made before five years. Many researchers argue that signs of ADHD are most pronounced between 5 and 12 years of age and during puberty (from about 14 years of age).
Although ADHD is rarely diagnosed in early childhood, some experts believe that There are a number of signs that suggest the likelihood of a baby having this syndrome. According to some researchers, the first manifestations of ADHD coincide with the peaks of a child’s psycho-speech development, that is, they most clearly manifest themselves at 1-2 years, 3 years and 6-7 years.
Children prone to ADHD often have increased muscle tone in infancy, experience problems with sleep, especially falling asleep, are extremely sensitive to any stimuli (light, noise, the presence of a large number of unfamiliar people, a new, unusual situation or environment), during When awake, they are often overly active and agitated.
What is important to know about a child with ADHD
1) Attention deficit hyperactivity disorder is considered to be one of the so-called borderline mental states. That is, in an ordinary, calm state, this is one of the extreme variants of the norm, but the slightest catalyst is enough to bring the psyche out of the normal state and the extreme variant of the norm has already turned into some kind of deviation. The catalyst for ADHD is any activity that requires increased attention from the child, concentration on the same type of work, as well as any hormonal changes that occur in the body.
2) Diagnosis of ADHD does not imply a delay in the child’s intellectual development. On the contrary, as a rule, children with ADHD are very smart and have fairly high intellectual abilities (sometimes above average).
3) The mental activity of a hyperactive child is characterized by cyclicity.. Children can work productively for 5-10 minutes, then the brain rests for 3-7 minutes, accumulating energy for the next cycle. At this moment, the student is distracted and does not respond to the teacher. Mental activity is then restored and the child is ready to work within the next 5-15 minutes. Psychologists say that children with ADHD have the so-called. flickering consciousness: that is, they can periodically “fall out” during activity, especially in the absence of motor activity.
4) Scientists have found that motor stimulation of the corpus callosum, cerebellum and vestibular apparatus of children with attention deficit hyperactivity disorder leads to the development of the function of consciousness, self-control and self-regulation. When a hyperactive child thinks, he needs to make some movements - for example, swing in a chair, tap a pencil on the table, mutter something under his breath. If he stops moving, he seems to “fall into a stupor” and loses the ability to think.
5) It is typical for hyperactive children superficiality of feelings and emotions. They They cannot hold a grudge for long and are not vindictive.
6) A hyperactive child is characterized by frequent mood changes- from stormy delight to unbridled anger.
7) The consequence of impulsivity in ADHD children is hot temper. In a fit of anger, such a child can tear up the notebook of a neighbor who offended him, throw all his things onto the floor, and shake out the contents of his briefcase onto the floor.
8) Children with ADHD often develop negative self-esteem- the child begins to think that he is bad, not like everyone else. Therefore, it is very important that adults treat him kindly, understanding that his behavior is caused by objective difficulties of control (that he does not want, but cannot behave well).
9) Often in ADHD children reduced pain threshold. They are also practically devoid of any sense of fear. This can be dangerous for the health and life of the child, as it can lead to unpredictable fun.
|
MAIN manifestations of ADHD Preschoolers Primary School Teenagers Adults |
How to recognize ADHD
Basic diagnostic methods
So, what to do if parents or teachers suspect that their child has ADHD? How to understand what determines a child’s behavior: pedagogical neglect, shortcomings in upbringing or attention deficit hyperactivity disorder? Or maybe just character? In order to answer these questions, you need to contact a specialist.
It’s worth saying right away that, unlike other neurological disorders, for which there are clear methods of laboratory or instrumental confirmation, There is no objective diagnostic method for ADHD. According to modern expert recommendations and diagnostic protocols, mandatory instrumental examinations for children with ADHD (in particular, electroencephalogram, computed tomography, etc.) are not indicated. There is a lot of work that describes certain changes in the EEG (or the use of other functional diagnostic methods) in children with ADHD, but these changes are nonspecific - that is, they can be observed both in children with ADHD and in children without this disorder. On the other hand, it often happens that functional diagnostics do not reveal any deviations from the norm, but the child has ADHD. Therefore, from a clinical point of view The basic method for diagnosing ADHD is an interview with parents and the child and the use of diagnostic questionnaires.
Due to the fact that with this violation the boundary between normal behavior and disorder is very arbitrary, the specialist has to establish it in each case at his own discretion(unlike other disorders where guidelines still exist). Thus, due to the need to make a subjective decision, the risk of error is quite high: both failure to identify ADHD (this especially applies to milder, “borderline” forms) and identification of the syndrome where it actually does not exist. Moreover, subjectivity doubles: after all, the specialist is guided by anamnesis data, which reflects the subjective opinion of the parents. Meanwhile, parental ideas about what behavior is considered normal and what is not can be very different and are determined by many factors. Nevertheless, the timeliness of diagnosis depends on how attentive and, if possible, objective people from the child’s immediate environment (teachers, parents or pediatricians) will be. After all, the sooner you understand the child’s characteristics, the more time it takes to correct ADHD.
Stages of diagnosing ADHD
1) Clinical interview with a specialist (child neurologist, pathopsychologist, psychiatrist).
2) Use of diagnostic questionnaires. It is advisable to obtain information about the child “from different sources”: from parents, teachers, a psychologist at the educational institution that the child attends. The golden rule in diagnosing ADHD is confirmation of the disorder from at least two independent sources.
3) In doubtful, “borderline” cases, when the opinions of parents and specialists regarding the presence of a child with ADHD differ, it makes sense video recording and its analysis ( recording of the child’s behavior in class, etc.). However, help is also important in cases of behavioral problems without a diagnosis of ADHD - the point, after all, is not the label.
4) If possible - neuropsychological examination a child, the purpose of which is to establish the level of intellectual development, as well as to identify often concomitant violations of school skills (reading, writing, arithmetic). Identification of these disorders is also important in terms of differential diagnosis, because in the presence of reduced intellectual capabilities or specific learning difficulties, attention problems in the classroom may be caused by the program not matching the child’s level of abilities, and not by ADHD.
5) Additional examinations (if necessary)): consultation with a pediatrician, neurologist, and other specialists, instrumental and laboratory tests for the purpose of differential diagnosis and identification of concomitant diseases. A basic pediatric and neurological examination is advisable due to the need to exclude “ADHD-like” syndrome caused by somatic and neurological disorders.
It is important to remember that behavioral and attention disorders in children can be caused by any common somatic diseases (such as anemia, hyperthyroidism), as well as all disorders that cause chronic pain, itching, and physical discomfort. The cause of “pseudo-ADHD” may also be side effects of certain medications(for example, biphenyl, phenobarbital), as well as a number of neurological disorders(epilepsy with absence seizures, chorea, tics and many others). The child's problems may also be due to the presence sensory disorders Here again, a basic pediatric examination is important to identify visual or hearing impairments that, if mild, may be underdiagnosed. Pediatric examination is also advisable due to the need to assess the general somatic condition of the child and identify possible contraindications regarding the use of certain groups of medications that can be prescribed to children with ADHD.
Diagnostic questionnaires
ADHD criteria according to DSM-IV classification
Attention disorder
a) is often unable to concentrate on details or makes careless mistakes when completing school assignments or other activities;
b) often have problems maintaining attention on a task or game;
c) problems often arise with organizing activities and completing tasks;
d) is often reluctant to engage in or avoid activities that require sustained attention (such as class assignments or homework);
e) often loses or forgets things needed to complete tasks or other activities (for example, a diary, books, pens, tools, toys);
f) is easily distracted by extraneous stimuli;
g) often does not listen when spoken to;
h) often does not adhere to instructions, does not complete assignments, homework or other work completely or to the proper extent (but not out of protest, stubbornness or inability to understand instructions/tasks);
i) forgetful in daily activities.
Hyperactivity - impulsiveness(at least six of the following symptoms must be present):
Hyperactivity:
a) cannot sit still, constantly moves;
b) often leaves his seat in situations where he must sit (for example, in class);
c) runs around a lot and “turns things over” where this should not be done (in adolescents and adults, the equivalent may be a feeling of internal tension and a constant need to move);
d) is unable to play quietly, calmly, or rest;
e) acts “as if wound up” - like a toy with the motor turned on;
f) talks too much.
Impulsiveness:
g) often speaks prematurely, without hearing the question to the end;
h) impatient, often cannot wait for his turn;
i) frequently interrupts others and interferes with their activities/conversations. The above symptoms must have been observed for at least six months, occur in at least two different environments (school, home, playground, etc.) and not be caused by another disorder.
Diagnostic criteria used by Russian specialists
Attention disorder(diagnosed when 4 of 7 signs are present):
1) needs a calm, quiet environment, otherwise he is not able to work and concentrate;
2) often asks again;
3) easily distracted by external stimuli;
4) confuses details;
5) does not finish what he starts;
6) listens, but seems not to hear;
7) has difficulty concentrating unless a one-on-one situation is created.
Impulsiveness
1) shouts in class, makes noise during the lesson;
2) extremely excitable;
3) it is difficult for him to wait his turn;
4) excessively talkative;
5) hurts other children.
Hyperactivity(diagnosed when 3 out of 5 signs are present):
1) climbs on cabinets and furniture;
2) always ready to go; runs more often than walks;
3) fussy, squirms and writhes;
4) if he does something, he does it with noise;
5) must always do something.
Characteristic behavior problems must be characterized by early onset (before six years) and persistence over time (manifest for at least six months). However, before entering school, hyperactivity is difficult to recognize due to the wide range of normal variations.
And what will grow from it?
What will grow from it? This question worries all parents, and if fate has decreed that you become the mother or father of an ADHD child, then you are especially worried. What is the prognosis for children with attention deficit hyperactivity disorder? Scientists answer this question in different ways. Today they talk about three most possible options for the development of ADHD.
1. Over time symptoms disappear, and children become teenagers and adults without deviations from the norm. Analysis of the results of most studies indicates that from 25 to 50 percent of children “outgrow” this syndrome.
2. Symptoms to varying degrees continue to be present, but without signs of developing psychopathology. These are the majority of people (50% or more). They have some problems in everyday life. According to surveys, they are constantly accompanied by a feeling of “impatience and restlessness,” impulsiveness, social inadequacy, and low self-esteem throughout their lives. There are reports of a higher frequency of accidents, divorces, and job changes among this group of people.
3. Developing severe complications in adults in the form of personality or antisocial changes, alcoholism and even psychotic states.
What path is prepared for these children? In many ways, this depends on us, adults. Psychologist Margarita Zhamkochyan characterizes hyperactive children as follows: “Everyone knows that restless children grow up to be explorers, adventurers, travelers and company founders. And this is not just a frequent coincidence. There are quite extensive observations: children who in elementary school tormented teachers with their hyperactivity, as they get older, are already interested in something specific - and by the age of fifteen they become real experts in this matter. They gain attention, concentration, and perseverance. Such a child can learn everything else without much diligence, and the subject of his hobby - thoroughly. Therefore, when they say that the syndrome usually disappears by high school age, this is not true. It is not compensated for, but results in some kind of talent, a unique skill.”
The creator of the famous airline JetBlue, David Neelyman, is happy to say that in his childhood he was not only diagnosed with such a syndrome, but also described it as “flamboyant”. And the presentation of his work biography and management methods suggests that this syndrome did not leave him in his adult years, moreover, that it was to him that he owed his dizzying career.
And this is not the only example. If you analyze the biographies of some famous people, it will become clear that in childhood they had all the symptoms characteristic of hyperactive children: explosive temperament, problems with learning at school, a penchant for risky and adventurous undertakings. It is enough to take a closer look around, remember two or three good friends who have succeeded in life, their childhood years, in order to draw a conclusion: a gold medal and a red diploma very rarely turn into a successful career and a well-paid job.
Of course, a hyperactive child is difficult in everyday life. But understanding the reasons for his behavior can make it easier for adults to accept a “difficult child.” Psychologists say that children are especially in dire need of love and understanding when they least deserve it. This is especially true for a child with ADHD who exhausts parents and teachers with his constant “antics.” The love and attention of parents, the patience and professionalism of teachers, and timely help from specialists can become a springboard for a child with ADHD into a successful adult life.
|
HOW TO DETERMINE WHETHER YOUR CHILD'S ACTIVITY AND IMPULSIVITY IS NORMAL OR HAS ADHD? ACTIVE CHILD - Most of the day he “does not sit still”, prefers active games to passive ones, but if he is interested, he can also engage in quiet activities. HYPERACTIVE CHILD
If you answered positively to at least three points, this behavior persists in the child for more than six months and you believe that it is not a reaction to a lack of attention and love on your part, then you have reason to think about it and consult a specialist. |
Oksana BERKOVSKAYA | editor of the magazine "Seventh Petal"
Portrait of a hyperdynamic child
The first thing that catches your eye when meeting a hyperdynamic child is his excessive mobility in relation to his calendar age and some kind of “stupid” mobility.
As a baby, such a child gets out of diapers in the most incredible way. ...It is impossible to leave such a baby on the changing table or on the sofa even for a minute from the very first days and weeks of his life. If you just gape a little, he will definitely twist somehow and fall to the floor with a dull thud. However, as a rule, all consequences will be limited to a loud but short scream.
Not always, but quite often, hyperdynamic children experience certain sleep disturbances. ...Sometimes the presence of hyperdynamic syndrome can be assumed in an infant by observing his activity in relation to toys and other objects (however, this can only be done by a specialist who knows well how ordinary children of this age manipulate objects). The exploration of objects in a hyperdynamic infant is intense, but extremely undirected. That is, the child throws away the toy before exploring its properties, immediately grabs another (or several at once) only to throw that one away a few seconds later.
...As a rule, motor skills in hyperdynamic children develop in accordance with age, often even ahead of age indicators. Hyperdynamic children, earlier than others, begin to hold their heads up, roll over onto their stomachs, sit, stand up, walk, etc. ... It is these children who stick their heads between the bars of the crib, get stuck in the playpen net, get tangled in duvet covers, and quickly and dexterously learn to remove everything that caring parents put on them.
As soon as a hyperdynamic child is on the floor, a new, extremely important stage begins in the life of the family, the purpose and meaning of which is to protect the life and health of the child, as well as family property from possible damage. The activity of a hyperdynamic baby is unstoppable and overwhelming. Sometimes relatives get the impression that it operates around the clock, almost without a break. Hyperdynamic children do not walk from the very beginning, but run.
...It is these children aged from one to two - two and a half years old who pull tablecloths with tableware onto the floor, drop televisions and Christmas trees, fall asleep on the shelves of empty wardrobes, endlessly, despite the prohibitions, turn on the gas and water, and also overturn pots with contents of different temperatures and consistencies.
As a rule, no attempts to reason with hyperdynamic children have any effect. They are fine with memory and speech understanding. They just can't help themselves. Having committed another trick or destructive act, the hyperdynamic child himself is sincerely upset and does not understand at all how it happened: “She fell on her own!”, “I walked, walked, climbed in, and then I don’t know,” “I didn’t touch it at all.” !
...Quite often, hyperdynamic children exhibit various speech development disorders. Some begin to speak later than their peers, some - on time or even earlier, but the problem is that no one understands them, because they do not pronounce two-thirds of the sounds of the Russian language. ...When they speak, they wave their arms a lot and confusedly, shift from foot to foot or jump in place.
Another feature of hyperdynamic children is that they do not learn not only from other people’s mistakes, but even from their own mistakes. Yesterday, a child was walking on the playground with his grandmother, climbed onto a high ladder, and could not get down. I had to ask the teenage boys to take it down from there. The child was clearly frightened when asked: “Well, are you going to climb this ladder now?” — he answers earnestly: “I won’t!” The next day, on the same playground, the first thing he does is run to that same ladder...
Hyperdynamic children are the ones who get lost. And there is absolutely no strength left to scold the child who is found, and he himself does not really understand what happened. “You left!”, “I just went to look!”, “Were you looking for me?!” - all this discourages, angers, makes you doubt the mental and emotional capabilities of the child.
...Hyperdynamic children, as a rule, are not evil. They are not able to harbor grudges or plans for revenge for a long time, and are not prone to targeted aggression. They quickly forget all insults; yesterday’s offender or the one offended today is their best friend. But in the heat of a fight, when already weak braking mechanisms fail, these children can be aggressive.
The real problems of a hyperdynamic child (and his family) begin with schooling. “Yes, he can do anything if he wants! All he has to do is concentrate - and all these tasks will be a breeze for him!” - nine out of ten parents say this or approximately this. The trouble is that a hyperdynamic child absolutely cannot concentrate. Sitting down for homework, within five minutes he is drawing in a notebook, rolling a typewriter on the table, or simply looking out the window behind which the older kids are playing football or preening the feathers of a raven. Another ten minutes later he will really want to drink, then eat, then, of course, go to the toilet.
The same thing happens in the classroom. A hyperdynamic child is like a speck in the eye for a teacher. He endlessly spins around, gets distracted and chats with his desk neighbor. ...He is either absent from work in class and then, when asked, answers inappropriately, or takes an active part, jumps on his desk with his hand raised to the sky, runs out into the aisle, shouting: “Me! I! Ask me! - or simply, unable to resist, shouts out the answer from his seat.
The notebooks of a hyperdynamic child (especially in primary school) are a pitiful sight. The number of errors in them competes with the amount of dirt and corrections. The notebooks themselves are almost always wrinkled, with bent and dirty corners, with torn covers, with stains of some kind of unintelligible dirt, as if someone had recently eaten pies on them. The lines in the notebooks are uneven, letters creep up and down, letters are missing or replaced in words, words are missing in sentences. The punctuation marks seem to appear in a completely arbitrary order - author's punctuation in the worst sense of the word. It is the hyperdynamic child who can make four mistakes in the word “more.”
Reading problems also occur. Some hyperdynamic children read very slowly, stumbling over every word, but they read the words themselves correctly. Others read quickly, but change endings and “swallow” words and entire sentences. In the third case, the child reads normally in terms of pace and quality of pronunciation, but does not understand what he read at all and cannot remember or retell anything.
Problems with mathematics are even less common and are usually associated with the child’s total inattention. He can solve a difficult problem correctly and then write down the wrong answer. He easily confuses meters with kilograms, apples with boxes, and the resulting answer of two diggers and two-thirds does not bother him at all. If there is a “+” sign in the example, the hyperdynamic child can easily and correctly perform subtraction, if there is a division sign, he will perform multiplication, etc. and so on.
A hyperdynamic child constantly loses everything. He forgets his hat and mittens in the locker room, his briefcase in the park near the school, his sneakers in the gym, his pen and textbook in the classroom, and his grade book somewhere in the trash heap. In his knapsack, books, notebooks, shoes, apple cores and half-eaten sweets coexist calmly and closely.
At recess, a hyperdynamic child is a “hostile whirlwind.” The accumulated energy urgently requires an outlet and finds it. There is no fight that our child will not get involved in, there is no prank that he will refuse. Stupid, crazy running around during recess or after-school activities, ending somewhere in the solar plexus of one of the members of the teaching staff, and appropriate indoctrination and repression is the inevitable ending to almost every school day of our child.
Ekaterina Murashova | From the book: “Children are “mattresses” and children are “catastrophes””
Over the past decade, the number of diseases commonly called hyperactivity, or scientifically called attention deficit disorder in children, has increased. How to understand: the baby is sick or pedagogically neglected?
Attention deficit hyperactivity disorder (ADHD) is a medical diagnosis defined as a neurological-behavioral developmental disorder. Characterized by difficulty concentrating, excessive motor activity, disregard for accepted social norms, aggressiveness, and inability to control emotions.
The first signs appear in preschool childhood, but according to the American Psychiatric Association, diagnosis is allowed only from the age of twelve. According to a 2006 study, 3–5% of the American population, including adults, have the disease.
A treatment for the neurological cause of the disorder has not been found. In 30% of children, symptoms disappear with age, or children adapt to them. In case of maladjustment, a decrease in intellectual abilities and perception of information is observed. There are methods for correcting behavioral deviations.

Since the 70s of the last century, there have been debates regarding the reality of this disease. Many public figures, politicians, doctors and parents consider it a fiction. The UN Committee on the Rights of the Child has confirmed an increase in misdiagnosis and has recommended more research into methods for recognizing ADHD.
The disorder is divided into 3 types:
- Attention deficit itself (ADHD - AD). Difficulty concentrating and remembering.
- Hyperactivity and impulsivity (ADHD - HI, ADHD - G). Motor disinhibition, restlessness, and thoughtlessness of actions are observed.
- Mixed type (ADHD - C). A combination of three signs.

Symptoms of the disease
Children who do not have this disease are often called hyperactive. The reason lies in the fact that signs of the disorder in small manifestations are characteristic of childhood: restlessness, difficulty concentrating with poor motivation, haste. And with a lack of education, they tend to worsen. This may be due to medical or parental error.
According to the 2007 guidelines for diagnosing ADHD:
- Diagnostics of behavior must take place in at least two environments (school – home – circle) of a child of senior school age;
- Long-term observation is necessary to determine the persistence of symptoms (at least six months);
- If the child’s development lags behind his peers;
- Behavioral disorders are accompanied by learning and communication difficulties.

Main signs of the disease
Absent-mindedness:
- It is difficult for a child to maintain attention on a task, to engage in activities that require long-term concentration, and is easily distracted.
- Often tries to avoid completing assignments that involve lengthy mental work (helping with housework, school homework).
- It is difficult to independently organize the implementation of some activity.
- Often loses necessary things, absent-minded.
- Cannot concentrate on details.
Impulsivity is insufficient control of actions when following instructions. An important symptom accompanying attention deficit in children:
- Quick reaction to the implementation of a task while ignoring or underestimating accompanying instructions.
- Inability to foresee the bad consequences of one's actions or circumstances.
- The desire to impress others (especially peers) with actions that are dangerous to their health and life (frequent poisoning, injuries).
Hyperactivity:
- Motor disinhibition. Constantly jumps around, fidgets in his chair, spins around.
- It is difficult for the child to sit in one place when necessary. During lessons he runs around the classroom.
- He plays loudly and is talkative.
Symptoms of ADHD appear starting in preschool age. The child is restless, makes many aimless movements, and unceremoniously interrupts adults. It’s difficult to get your little one to prepare for school. Having sat down to study under my mother’s pressure, he is constantly distracted.

School-age children have problems mastering material due to their low ability to concentrate. Academic performance is below average, difficulties in relationships with peers. Conducting a lesson in a classroom with a child with attention deficit disorder is difficult. He constantly distracts others, spins around, interrupts the teacher, and is in a hurry to complete the task. Books and notebooks are forgotten in class. Despite their disinhibited behavior, younger schoolchildren do not show aggression.
Adolescence changes symptoms. External impulsiveness turns into internal anxiety and fussiness. The inability to independently plan time and organize activities leads to irresponsibility. Poor academic performance and problems communicating with classmates affect self-esteem, which leads to depression and short temper. The desire to occupy a significant position among peers can push one to take thoughtless risks, often resulting in injuries and bruises.
If the teenager does not outgrow the disease, it progresses into adulthood. Emotional instability and irritability persist. Chronic lack of punctuality, forgetfulness, inability to complete initiatives, and high sensitivity to criticism make him a bad employee. Low self-esteem prevents you from realizing your potential. People suffering from this disease often find an outlet in various addictions: alcohol, drugs. If you don’t engage in self-development, you risk finding yourself at the bottom of your life.

Causes of pathology
Experts have not yet clearly established the triggering factors for ADHD. Presumable ones are:
- Genetic background. It is assumed that the disorder is congenital and is associated with a malfunction of the central nervous system. This is what scientists see as the neurological root of the disease.
- Deteriorating ecology. Air poisoning from exhaust gases, water pollution from harmful household chemicals.
- Features of the course of pregnancy. Infectious and chronic diseases of the mother, alcohol consumption, smoking.
- Complications during childbirth: long, rapid, stimulation of labor, intoxication by anesthesia, entanglement of the fetus with the umbilical cord.
- Illnesses in the first year of life, accompanied by high fever, and taking potent medications.

Diagnostic methods
The medical community has been debating for half a century about effective ways to recognize ADHD. Scientists at Canada's McMaster University have confirmed that there are currently no specific tests or medical equipment that directly diagnose ADHD. In addition, the criteria for diagnosing the disease have changed during the existence of the diagnosis and differ in different countries.
American psychiatrists use two scales: Connors and Yale-Brown, which ask parents or teachers to evaluate the child’s behavior according to parameters characteristic of the disorder: inattention, hyperactivity and impulsivity. However, experts who criticize the diagnostic methods argue that the assessment of behavior on these scales is too biased, and the diagnostic criteria are so vague that it is possible to diagnose ADHD in any healthy child with “uncomfortable” behavior.
To avoid medical errors, consultation with several specialists is necessary, including a pediatrician, psychologist and pediatric neurologist. Additional medical examinations will be required: MRI of the brain, Doppler sonography, EEG, which will be the basis for a psychiatrist’s diagnosis of ADHD.

Treatment of the disease
To correct attention deficit in children, an integrated approach is required, including the eradication of neuropsychological and behavioral problems. Taking into account the characteristics and type of ADHD of the child, a personal rehabilitation program is selected. With timely consultation with a specialist and treatment, it is possible to reduce the symptoms of ADHD until recovery.
Drug therapy
It should be noted that the prescription of pharmacological correction is acceptable in cases where restoration of cognitive functions cannot be achieved with non-drug treatment.
Taking medications to improve brain function in children with attention deficit disorder is a fairly common practice in the United States. Medicines are divided into several groups:
- Psychostimulants (Ritalin (methylphenidate), Amphetamine, Dexamphetamine). They have a powerful stimulating effect on the central nervous system: improve concentration, reduce manifestations of impulsivity. In the United States, Ritalin is commonly used to treat ADHD, although there is no evidence of effectiveness. Many experts consider it controversial, since long-term use of Ritalin leads to the development of psychosis, paranoid and schizophrenic tendencies (visual and auditory hallucinations, aggressiveness), and is addictive. An Australian study involving 2868 families and lasting 20 years showed the ineffectiveness of psychostimulant treatment for ADHD. In a number of countries, including Russia, methylphenidate (Ritalin) is prohibited.
- Antidepressants: Imipramine, Thioridazine, Desipramine. Significantly improve attention, reduce hyperactivity, but have side effects on physical health with long-term use.
- Nootropic drugs (Nootropil, Cerebrolysin, Piracetam). Neurometabolic stimulants that affect the cerebral cortex and enhance cognitive processes. They are considered low-risk psychopharmacological drugs, but can cause complications. Widely used in post-Soviet countries.

A significant disadvantage of drug therapy for ADHD is the short-term results of treatment: the child’s condition improves only while taking the drug and has no effect on recovery at all. The use of psychostimulants by adolescents with attention deficit disorder develops a tendency to take drugs.
Non-pharmacological therapy
ADHD can be treated without the use of medications. There are two non-drug methods for correcting the neurological side of the disorder:
- Neuropsychological approach. Claims that certain physical exercises affect the functioning of the cortical structures of the brain, activate and fill mental processes with energy. Based on the teachings of A.R. Luria on the “neuropsychological developmental loop”. This support for children with attention deficit helps to develop self-control, arbitrariness, and increase learning efficiency.
- Syndromic method. Restoration of the cervical spine damaged due to birth injuries, which normalizes blood supply to the brain.
In addition to the treatment methods described above, experts recommend:
- Yoga classes, meditation. Helps you relax, reduces impulsivity, improves blood supply to the whole body, including the brain.
- Special diet. Elimination of sugar, allergens, caffeine.

Behavior correction for ADHD consists of the following methods:
Cognitive psychotherapy is the most effective treatment used in the correction of mental disorders (neuroses, phobias, depression). Helps children with attention deficit problems who have problems communicating with peers successfully socialize. Impulsivity coupled with a lack of interaction skills leads to rejection, which exacerbates isolation.
Therapy includes personal and group sessions. Communication skills training helps develop the following communication abilities: the ability to build relationships, resolve conflicts, understand others, and control negative emotions. To successfully master the skills, you must attend at least 20 classes in a group consisting of 6–8 people. Personal cognitive behavioral therapy breaks up ineffective patterns of action and thinking. Helps children with attention deficit to reinforce the desired behavior.
- Family psychotherapy. Must be present in the treatment of ADHD in children. Spent with the whole family. Parents face their feelings of guilt for a “not that kind” child and learn to react correctly in life’s circumstances.

For attention deficit disorder in children, treatment must involve doctors, parents and teachers. The greatest burden falls on the family, whose members must have a good knowledge of the characteristics and methods of treating ADHD, and create conditions at home that are conducive to the child’s recovery:
- Love. Show tenderness and care. The baby needs to feel the support of loved ones.
Important! The feeling of pity is a bad ally. Do not free the student from various household chores, fueling his “special” status. He will begin to feel sorry for himself, which will negatively affect the dynamics of treatment.

Together, we can correct the child’s behavior and help him recover.
A child's behavior often makes parents worry. But this is not about ordinary licentiousness or disobedience, as it seems at first glance to outsiders. In some cases, everything is much more complicated and serious. Such behavioral characteristics can be provoked by a special state of the nervous system. In medicine, it is called hyperactivity disorder and is usually paired with attention deficit disorder. Shortened form? ADHD.
Hyperactive children cause parents a lot of worries
What does it mean?
Literally, the prefix “hyper” means “excessively.” It is difficult for a child to play with the same toys not just for a long time, but even for several minutes. The baby cannot remain still for more than 10 seconds.
Is there a shortage? This is an insufficient level of concentration and ability to concentrate in a child, which affects constant excitement and rapid change of objects of interest.
Now every parent who reads the meaning of the terms will think: “My child is very restless, asks questions all the time, and can’t sit still. Maybe there’s something wrong with him and you need to see a doctor immediately?”
 Definition of hyperactivity
Definition of hyperactivity In fact, children should be in constant motion, because they learn about the world and themselves in it. But sometimes it is difficult for a child to complete assigned tasks, calm down in time, and even just stop. And here it is necessary to think about the reasons.
Is deviation from the norm a problem?
First of all, we emphasize that we use the word “norm” conditionally. It implies a set of fixed skills of typical behavior. However, any deviations from the prescribed parameters should not be perceived as the end of the world. It is very important for parents not to despair, but to understand the situation and help the child.
Main task? identify the baby’s peculiarities in a timely manner, do not miss the moment and learn to properly manage the situation.
Early detection of hyperactivity syndrome
As practice shows, before school age a child’s characteristics are rarely identified, although symptoms are present almost from birth, as they are genetically determined. Teachers are now paying more attention to specifics. And some manifestations are noticeable even before 3 years, in particular:
- a child under one year of age moves his arms and legs without stopping during the waking period;
- it is difficult for a child to play with one toy even for a short period of time;
- the baby is extremely emotional, easily becomes hysterical, it is difficult for him to calm down, stop crying, yelling, etc.;
- It seems that he does not respond to comments at all.
What parents should pay attention to
 Lack of attentiveness is a sign of ADHD
Lack of attentiveness is a sign of ADHD Psychological disorders associated with insufficient attention and hyperactivity include three categories:
- Direct inattention.
- Increased activity.
- Unusual impulsiveness.
Each category has a number of behavioral characteristics. Problems are predominantly identified in a comprehensive manner. Therefore, it is important to understand that you cannot focus only on one condition. In order to establish a diagnosis, there must be matches in at least three positions.
Specific signs of attention problems
The following circumstances indicate attention deficit disorder in children:
- difficulty focusing on details, individual objects, pictures;
- difficulties with gaming activities;
- elementary tasks remain unfulfilled, for example, “Bring it!”, “Tell me!”, “Do it in half an hour,” etc.;
- unwillingness to put in any effort and fulfill responsibilities;
- poor self-organization in everyday life: the child is constantly late, does not have time to do anything, loses his things;
- during a group conversation or conversation, it seems that he is not listening at all;
- a long process of memorization, but instant distraction by foreign objects;
- quick switch to another occupation;
- loss of interest in previous hobbies and interests.
Hyperactivity conditions
There is an acceptable number of signs to determine the normal development of a child, but it should not exceed three of the following characteristics:

Definition of impulsivity
Even one of the following characteristics is a cause for concern:
- the child answers questions prematurely;
- unable to wait his turn in games or other situations;
- interferes in other people's conversations.
Other characteristics
 Impulsivity and excessive emotionality are a sign of ADHD
Impulsivity and excessive emotionality are a sign of ADHD Violations are observed not only in psychological characteristics, but also in medical, physiological, and emotional ones. Closer to 5 years of age, a child may exhibit symptoms of the following nature:
- general state of the emotional sphere: constant anxiety, stuttering, difficulty formulating speech clearly and correctly, lack of restful sleep and rest;
- motor dysfunction: motor and vocal tics. The child involuntarily makes sounds, waves his arms or legs;
- physiological conditions and concomitant medical diseases: persistent allergic reactions, intestinal and urinary disorders, epileptic manifestations.
 Causes of hyperactivity
Causes of hyperactivity What to do?
After a diagnosis of hyperactivity and attention deficit disorder is made, parents reach a dead end and ask the question: “What will happen now? How to behave? How to help and treat a child correctly?
Indeed, the problem requires increased attention and considerable effort on the part of both close relatives, educators, teachers, and the entire environment of the child. Therefore, you need to be patient and have a qualified approach to education.
 Changes in the brain of a hyperactive child
Changes in the brain of a hyperactive child Modern medicine uses many options for managing diagnosis. But they all must be used in combination. In order of importance, they include:
- Psychological home help for a child.
- Treatment with medications and folk remedies.
- Nutrition and diet.
Behavioral therapy
Eliminating hyperactivity in a child, first of all, involves creating a special atmosphere in the family. Only close people can really help a child and teach him to control himself. If your relatives do not have specific teaching skills, you can seek recommendations from a qualified psychologist.
 Advice for parents - what to do
Advice for parents - what to do To improve behavior, psychologists advise:
- Create a comfortable atmosphere in the family. The child should not hear insults or curses.
- Emotional stress in a child has a bad effect on his psychological state. Therefore, he should always feel the love and attention of his parents.
- Find the positive aspects of studying, in every way help your child behave well at home, in kindergarten, and then at school.
- At the slightest feeling of fatigue, the baby must be given the opportunity to rest, relax, and then he can begin classes or studies again.
- Tell educators, school psychologists and teachers about the problem. Together they will contribute to further adaptation in society.
How to treat attention deficit disorder in children
The child is treated by psychologists and neurologists. They prescribe drugs that can increase or change the functioning of the corresponding areas of the brain. It is only important to find a truly competent specialist and trust him.
The following medications are usually prescribed:

Nutrition and Diet Issues
Children diagnosed with ADHD are advised to follow a special diet. Because doctors believe that some foods and drinks aggravate the condition of young patients.
 The right diet is the basis for treating ADHD
The right diet is the basis for treating ADHD - Almost completely eliminate the consumption of sugar and sweets;
- Avoid artificial flavors, sweeteners, dyes and unnatural fat-containing ingredients (sweets, baked goods, sausages, etc.);
- Eat more whole grains and bran;
- Consume as much natural food as possible, home-cooked dishes;
- Diversify your child’s vegetable and fruit menu, fill it with different varieties of cabbage, carrots, apples, citrus fruits, apricots, nuts, etc. All food should be beautiful and healthy, without harmful synthetic additives.
Children have a strong emotional connection with their parents. Therefore, the correct behavior of those closest to you and relatives plays an important role in managing the diagnosis of ADHD.
Adhere to the following rules:

Does the problem go away with time?
With the right approach and treatment, manifestations of hyperactivity and attention deficit in a child decrease over time and become almost invisible by adolescence.
 Possible consequences of ADHD
Possible consequences of ADHD However, it should be understood that the diagnosis cannot completely disappear. It will go into a hidden form or transform, occasionally reminding itself of a quick change of mood, depression or the inability to do one thing. Therefore, the main task of parents and teachers is to teach the child to independently control his emotions and behavior, to use willpower and determination.
Remember! Children with attention deficit hyperactivity disorder really need to constantly feel love and affection. They may not always be attentive themselves, but they really want other people to treat them with understanding and attentiveness.
Patience, support and diligence can change the attitude towards special and unique members of society!
Similar materials

Attention deficit hyperactivity disorder (ADHD) is a neurobehavioral disorder that is typically characterized by the following symptoms:
Inattention;
- distractibility;
- impulsiveness;
- hyperactivity.
Kinds
Attention deficit hyperactivity disorder is divided into three subtypes:
Predominantly hyperactive or impulsive type. Behavior is marked by hyperactivity and impulsivity, but not inattention;
- mostly inattentive type. Behavior is marked by inattention, but not hyperactivity and impulsivity;
- combined type. A combination of symptoms of hyperactivity and impulsivity - with symptoms of inattention. This is the most common type of attention deficit hyperactivity disorder.
in children
Attention deficit hyperactivity disorder is sometimes described as a decline in brain function. It refers to the cognitive abilities needed to plan, organize, and complete tasks. Deficiencies in executive function can cause the following problems:
Inability to store information in short-term memory;
- violation of organization and planning skills;
- difficulties in establishing and using behavioral guidelines - such as choosing a strategy and monitoring tasks;
- overwhelming inability to cope with emotions;
- inability to effectively move from one mental activity to another.
Symptoms of attention deficit hyperactivity disorder in children
- Hyperactivity. The term "hyperactive" is often misleading because to some it suggests that the child is in constant, non-stop motion. However, boys with ADHD may have the same level of activity when playing a game, for example, as children without the syndrome. But when a child receives increased attention, his brain increases motor activity. In a busy environment - a classroom or a crowded store - children with ADHD are often distracted and overreact. They can take goods from shelves without asking their parents, beat people - in a word, everything gets out of control for them, resulting in unstable and strange behavior.
- Impulsiveness and hysteria. Tantrums, which are normal in young children, tend to be exaggerated in children with ADHD and are not necessarily related to a specific negative event.
- Attention and concentration. Children with attention deficit hyperactivity disorder tend to become distracted and inattentive to their environment (such as a large classroom). In addition, they are inattentive when the atmosphere is calm or boring. Instead, they may have a kind of “superfocus” when engaged in highly stimulating activities (such as video games or very specific interests). Such children can even become overly attentive - they are so absorbed in an activity that interests them that they are completely unable to change the direction of their attention.
- Impaired short-term memory. An important feature of attention deficit hyperactivity disorder, including in learning, is impairment of working (or short-term) memory. People with ADHD cannot hold groups of sentences and images in their minds long enough to extract clear, coherent thoughts. They are not necessarily inattentive. A person with ADHD may be unable to remember a complete explanation (such as a homework assignment) or be unable to complete processes that require sequential memorization (such as a model of a building). Children with ADHD are often attracted to activities (TV, computer games, vigorous individual sports) that do not overload working memory or produce distractions. Children with ADHD do not differ from other children in long-term memory.
- Inability to manage time. Children with ADHD may have difficulty being everywhere on time and managing time to complete certain tasks (which may overlap with short-term memory problems).
- Lack of ability to adapt. Children with ADHD often have great difficulty adapting to even minor changes in routines such as getting up in the morning, putting on shoes, eating new foods, or changing their sleep patterns. Any situation where anything changes can cause them to have a strong and noisy negative reaction. Even when they are in a good mood, they may suddenly become hysterical if they encounter an unexpected change or disappointment. These children can focus their attention directly on cues in a specific location, but have difficulty shifting their attention to anything else.
- Increased sensitivity and sleep problems. Children with ADHD are often hypersensitive to objects, sounds, and touch. They may complain of excessive stimuli that seem minor or mild to others. Many children with ADHD often have trouble sleeping during the night.
Attention deficit hyperactivity disorder in adults
Attention deficit hyperactivity disorder is a chronic condition that begins in childhood. Adult attention deficit hyperactivity disorder is a continuation of the symptoms of childhood attention deficit hyperactivity disorder.
Symptoms of attention deficit hyperactivity disorder in adults
- Mental disorders. About 20% of adults with ADHD also have major depression or bipolar disorder. Up to 50% have anxiety disorders. Bipolar disorders can be very difficult to distinguish from ADHD, not only in adults, but also in children.
- Disorders accompanying learning. About 20% of adults with attention deficit hyperactivity disorder have a learning disorder. These are usually dyslexia and auditory processing problems.
- Impact on work. Compared to adults without ADHD, those with ADHD tend to have lower levels of education, earn less money, and, as a result, are more likely to be fired.
- Substance abuse. About 1 in 5 adults with ADHD also struggle with substance abuse. Research shows that teens with ADHD are twice as likely to smoke cigarettes than their peers who do not have ADHD. Smoking during adolescence is a risk factor for the development of substance abuse in adulthood.
Causes attention deficit hyperactivity disorder
- Brain structure. Studies using modern imaging techniques show differences in the size of certain parts of the brain in children with attention deficit hyperactivity disorder compared to children without ADHD. Areas with changes include: prefrontal cortex, caudate nucleus, globus pallidus, and cerebellum;
- Brain chemicals. Increased activity of certain brain chemicals in the prefrontal cortex may contribute to ADHD. The chemicals dopamine and norepinephrine are of particular interest. Dopamine and norepinephrine are neurotransmitters (chemical messengers in the brain) that influence mental and emotional functioning. They also play a role in reward response. This reaction occurs when a person experiences pleasure in response to certain stimuli (such as food or love). Research shows that increased levels of the brain chemicals glutamate, glutamine and GABA - interact with dopamine and norepinephrine;
- Genetic factors. Genetic factors likely play an important role in ADHD. Families of children with ADHD (boys and girls) have a much higher percentage of ADHD, as well as antisocial anxiety and substance abuse disorders, than families without children with attention deficit hyperactivity disorder. Some twin studies suggest that up to 90% of children diagnosed with ADHD share it with their twin. Most research is being done on the underlying genetic mechanisms of the neurotransmitter dopamine. Changes in genes that regulate specific dopamine receptors have been found in a large number of people with attention deficit hyperactivity disorder.
Risk factors attention deficit hyperactivity disorder
- Floor . ADHD is diagnosed more often in boys than in girls. Boys are more likely to have combined ADHD. Girls are more likely to have a predominantly inattentive type;
- Family history. A child who has a parent or sibling with attention deficit hyperactivity disorder has an increased risk of also getting ADHD;
- Environmental factors. Some studies show that maternal alcohol consumption, drug abuse and smoking during pregnancy can lead to the development of attention deficit hyperactivity disorder in the child. Low birth weight may be associated with ADHD. Environmental exposure to lead before age 6 may also increase the risk of ADHD;
- Nutrition factors. Several dietary factors have been studied in relation to ADHD, including sensitivity to certain dietary chemicals, deficiencies in fatty acids (compounds from fats and oils) and zinc, and sensitivity to sugar. However, no clear evidence has emerged that any of these dietary factors imply risk factors for the development of ADHD.
Diagnostics attention deficit hyperactivity disorder
Diagnosis of attention deficit hyperactivity disorder in children
There is no single test to diagnose ADHD. The doctor does a physical examination of the child to make sure that an underlying medical condition is not causing ADHD symptoms. However, the diagnosis of ADHD is based primarily on the child's observations and questionnaire, as well as the behavior patterns of the ACT (Activity and Optimism Scale). The pediatrician may refer a child with SAD to a psychiatric hospital, where doctors have experience working with childhood disorders such as ADHD.
- History of behavior. The doctor will ask questions for a detailed history of the child and will identify the severity of his behavior. Parents should describe specific problems encountered with the child, developmental ADHD, family history of ADHD, and any recent changes in family life that may have affected the child. The doctor will find out everything important about the child, about all the details of his life outside the home: written reports from teachers, school psychologists, guardians or others related to the child, etc.
- Medical examination. The physical examination should include a hearing test to rule out any hearing problems in the child. The doctor should ask about a history of medical problems, including allergies, sleep disturbances, poor vision, and chronic ear infections.
To be diagnosed with ADHD, at least six of the following symptoms must have been present for at least 6 months (9 months in preschool children).
Symptoms of inattention (at least six of them should be present):
The child is often unable to pay close attention to detail or makes careless mistakes;
- often has difficulty maintaining attention in tasks or games;
- often does not seem to listen when people speak directly to him;
- often does not complete tasks or assignments;
- has difficulty organizing tasks and activities;
- avoids or dislikes tasks that require sustained mental effort;
- often loses things necessary for tasks or activities;
- often easily distracted by extraneous stimuli;
- often forgetful in daily activities.
Symptoms of hyperactivity and impulsivity (at least six of these must be present):
Often fidgets or squirms while sitting;
- has difficulty sitting when required;
- frequently works or frequently rises in inappropriate situations;
- cannot play calmly;
- often on the move;
- often talks too much;
- often blurts out answers to questions before they have been asked completely;
- has difficulty waiting for his turn;
- often interrupts others.
Based on these symptoms, a child may be diagnosed with a predominantly inattentive type of ADHD, a predominantly hyperactive-impulsive type of ADHD, or a combined type of ADHD.
Diagnosis of attention deficit hyperactivity disorder in adults
Childhood attention deficit hyperactivity disorder can affect children between the ages of 4 and 18 years. ADHD in adults always occurs as a continuation of childhood ADHD. Symptoms that begin in adulthood are caused by factors unrelated to ADHD.
Attention deficit hyperactivity disorder in adults is often difficult to diagnose. The doctor should ask about the history or symptoms of childhood ADHD. The patient may ask parents or former teachers to provide school records or other useful information about him. The doctor will ask the patient questions about the following types of symptoms:
Inattention and problems with memory (the patient may forget or lose things, being absent-minded, not finishing things, underestimating time, the order of things, he has problems when starting or changing work, halfway through its completion);
- hyperactivity and restlessness (the patient is always on the go, fussy, slightly bored, strives for an active and fast pace in work and activities);
- impulsiveness and emotional instability (the patient says things without thinking, interrupts others, gets irritated with other people, is easily disappointed, his mood is unpredictable, rash);
- problems with self-esteem (the patient avoids new tasks, he develops confidence in others, but not in himself).
Complications attention deficit hyperactivity disorder
Attention deficit hyperactivity disorder can be a problem for children and their loved ones.
- Emotional problems. Children with attention deficit hyperactivity disorder, especially those who also have anxiety or depressive disorders, typically suffer from low self-esteem.
- Social problems. ADHD can affect children in their relationships with peers. Children with ADHD may have difficulties with social skills and related behavior that can lead to bullying (both as a victim and as a perpetrator) and rejection. Impulsivity and aggression can lead to fights and negative interactions with other children. Children with attention deficit hyperactivity disorder and high levels of aggression may be at higher risk for delinquent behavior (an individual's antisocial, unlawful behavior embodied in his or her misconduct—actions or inactions that harm individuals and society as a whole) during adolescence and criminal activity. in adulthood.
- Risk of injury. Impulsivity in young people with ADHD may put them at risk of not thinking about consequences. Children with attention deficit hyperactivity disorder have an increased risk of accidents and injuries. For example, a child with ADHD may not be tested on their ability to react to oncoming traffic while riding a bicycle or whether they can participate in high-risk, physically demanding activities. All of these problems of children with ADHD carry over into their adult lives.
- Alcohol or drug abuse. Research shows that youth with ADHD—specifically conduct or mood disorder—have an above-average risk of substance abuse that begins at a young age. Biological factors associated with ADHD may make these individuals susceptible to substance abuse. Many of these young people can recover themselves from this condition.
- Problems with learning. Although speech and learning disorders are common in children with ADHD, they do not affect their intelligence. People with attention deficit hyperactivity disorder have the same IQ (intelligence quotient) range as the general population. Many children with ADHD struggle in school. Some evidence suggests that inattention may be a major factor in poor academic performance in these children. Difficulties in reading can also cause problems for them. Poor academic performance can affect a child's self-esteem and self-confidence, and influence various social problems in relationships with peers.
- Impact on the family. The time and attention required to address problems in children with ADHD can alter internal family relationships and lead to conflicts with parents and siblings.
Other disorders associated with ADHD
Some disorders may mimic or accompany ADHD. Many of these disorders require other treatments and must be diagnosed separately, even if they co-occur with ADHD.
- Oppositional defiant disorder (THIEF). It is often associated with attention deficit hyperactivity disorder. The most common symptom of this disorder is negative, defiant, and hostile behavior toward authority figures that lasts for more than six months. In addition to inattention and impulsive behavior, these children exhibit aggression, frequent tantrums, and display antisocial behavior. A significant number of children with VOR disorder also have anxiety and depression, which should be treated separately. Many children who develop VOR at an early age go on to develop conduct disorder.
- Behavior disorder. Some children with ADHD also have conduct disorder, which is described as a complex group of behavioral and emotional disorders. It includes aggression towards people and animals, destruction of property, seduction, deception, theft and general violation of social rules.
- Developmental disorder. The developmental disorder is rare and is usually characterized by autistic behavior, flapping hands, repetitive statements, and slow speech and motor development. If a child who has been diagnosed with ADHD does not respond to treatment, parents may view it as a developmental disorder that often responds to antidepressants. Some such children may also benefit from stimulant medications.
- Hearing disorders. Hearing problems can mimic symptoms of ADHD and should be assessed during diagnosis. Hearing disorders are another condition that can affect children's ability to process auditory information. Children with this type of disorder have normal hearing, but something in their brain does not allow them to filter out background noise and differentiate between similar sounds. A hearing disorder may be misdiagnosed as ADHD and may co-occur with it.
- Bipolar disorder. Children diagnosed with attention deficit disorder may also have bipolar disorder, which used to be called manic depression. Bipolar disorder is characterized by episodes of depression and mania (with symptoms of irritability, rapid speech, and blackouts). Both disorders often cause inattention and distractibility and can be difficult to tell apart, especially in children. In some cases, ADHD in children and adolescents may be a marker for developing bipolar disorder.
- Anxiety disorders. Anxiety disorders often accompany ADHD. Obsessive-compulsive disorder is a specific anxiety disorder that shares many of the characteristics of ADHD, with some genetic components. Young children who have experienced a traumatic event (including sexual or physical abuse or neglect) may exhibit characteristics of ADHD, including impulsivity, emotional outbursts, and oppositional behavior.
- Sleep disturbance. Sleep disorders often associated with attention deficit hyperactivity disorder include insomnia, restless leg syndrome, and sleep apnea (sleep breathing disorder).
Diseases with similar symptoms
- Tourette's syndrome and other genetic disorders. Several genetic disorders cause ADHD-like symptoms, including Tourette's syndrome. For many patients with Tourette's syndrome and ADHD, some of the treatments are similar.
- Lead poisoning. Children who ingest even small amounts of lead may exhibit symptoms similar to attention deficit hyperactivity disorder. The child may be easily distracted, disorganized, and unable to think logically. The leading cause of lead poisoning is exposure to lead paint, especially in older homes that are poorly maintained.
Ltreatment attention deficit hyperactivity disorder
Attention deficit hyperactivity disorder is considered a chronic disease that requires long-term, ongoing monitoring and adjustment of symptoms, medications, and other treatment programs. Although symptoms may improve over time, ADHD does not usually “go away.” Patients can, however, learn to control their condition through behavioral techniques, which are often supported by medication.
Treatment for attention deficit hyperactivity disorder does not completely reverse the condition, but focuses on controlling symptoms and improving the person's functioning. Treatment usually involves a combination of psychostimulants. These are usually: Methylphenidate (Ritalin) and behavioral therapy (other drugs may also be used for older children and adults). Treatment often involves a systemic approach that includes the child's pediatrician, other health care providers, parents, and teachers.
For preschool-aged children (ages 4-5), behavioral therapy provided by parents and teachers should be considered first. For many children, behavior therapy alone results in significant improvement. If further treatment is necessary and the benefits seem to outweigh the risks, the doctor may prescribe the stimulants Methylphenidate (Ritalin, etc.);
- For school-age children (ages 6-11), a combination of medication, stimulant and behavioral therapy is needed. Alternatives to stimulant medications, in order of recommendation: Atomoxetine (Strattera), Guanfacine (Tenex), or Clonidine (Catapres);
- Adolescents (aged 12-18 years) should be treated with medications and, if necessary, behavioral therapy. Some patients at this age may be able to temporarily stop taking their medications. The doctor should closely monitor the child during this time. Teens should also have their medication doses adjusted as they grow and change during puberty;
- treatment of adult ADHD. As with children, treatment for adults with ADHD is a combination of medications and psychotherapy. For medications, stimulants or non-narcotic stimulants, Atomoxetine (Strattera) is usually the first line treatment, and with antidepressants it is a secondary option. Most stimulant medications, including Atomoxetine, are approved for use in adults with ADHD. Adults who have heart problems or risk factors should be aware of the cardiovascular risks associated with ADHD treatment.
Medicines for the treatment of attention deficit hyperactivity disorder
Several types of medications are used to treat attention deficit hyperactivity disorder:
- Psychostimulants. These are the main drugs used to treat attention deficit hyperactivity disorder. Although these drugs stimulate the central nervous system (CNS), they have a calming effect on people with ADHD. These drugs include methylphenidate and amphetamine. These drugs increase dopamine, a neurotransmitter important for cognitive functions such as attention.
- Alpha-2 agonists. Alpha-2 agonists stimulate the neurotransmitter norepinephrine, which may be important for concentration. These include guanfacine and clonidine. Alpha-2 agonists are used for Tourette's syndrome and may be useful when other medications fail to help children with attention deficit hyperactivity disorder with severe impulsivity and aggression. These drugs may be prescribed in combination with stimulants.
- Antidepressants. Because antidepressants work as well as behavioral therapy, doctors recommend that patients first try psychotherapy before using antidepressants.
Behavior correction
Behavioral management techniques for a child with ADHD are not immediately clear to most parents and teachers. To get to know them, they may all need help from qualified psychologists and health professionals or ADHD support groups. The idea of changing the behavior of a very energetic and stubborn child is daunting at first. It is useless and harmful to force a child with attention deficit hyperactivity disorder to be like most other, healthy children. It is possible, however, to limit his destructive behavior and instill in a child with ADHD a sense of self-worth that will help him overcome all the negativity.
Raising a child with ADHD, like raising any child, is a difficult process. A child's self-esteem will develop as the child's ability to step back and think about the consequences of a possible action increases, and then to control the action before taking it. But it doesn't happen quickly. A growing child with ADHD is different from other children in very specific ways and presents challenges at any age.
Parents must first create their own tolerance levels. Some parents are calm and can accept a wide range of their child's behavior, while others cannot. Helping your child achieve self-discipline requires compassion, patience, love, and loyalty.
- Setting agreed rules for the child. Parents should be as consistent as possible in their approach to the child, rewarding good behavior and discouraging destructive behavior. Rules of conduct for a child should be clearly defined, but flexible enough to include harmless features. It is important to understand that children with ADHD have a much harder time adapting to change than other children. Parents should create predictable situations and provide a neat and stable environment at home (especially in the children's room).
Also, through useful literature and work with psychologists and doctors, parents should learn to competently manage the aggression of their child suffering from attention deficit hyperactivity disorder .
In addition, parents of children with attention deficit hyperactivity disorder absolutely need to learn how to reward such children for any good and calm behavior. There are many ways.
- Improved concentration and attention. Children with ADHD perform significantly better on academic tasks when they have an interest in the subject. Parents should be on the lookout for all activities that keep the child's concentration. Options include swimming, tennis, and other sports that focus attention and limit peripheral stimulation (children with ADHD may have difficulty with team sports that require constant alertness, such as soccer or basketball).
- Interaction with the school. Even if one parent successfully manages their child at home, the child with ADHD often has difficulties at school. The ultimate goal of any educational process is the happy, prosperous and healthy social integration of children with attention deficit hyperactivity disorder with their peers.
- Teacher training. Any teacher must be prepared for the behavioral characteristics of children with attention deficit hyperactivity disorder in order to competently manage these children. They, like the parents of such children, need to study the relevant medical, pedagogical and other literature and also actively consult with psychologists and doctors on this matter.
- The role of parents in school. Parents can help their child by talking to the teacher before the start of the school year about their child's situation. The primary task for parents is to develop a positive, rather than aggressive, impatient, or overly strict attitude of the teacher towards the child. Finding a mentor who can help your child study after school can also be very helpful.
- Special education programs. High quality special education can be very helpful in improving a child's learning and self-esteem. However, programs vary in their ability to provide quality education. Parents should be aware of some restrictions and issues with special education:
Special education programs in a normal school setting often increase a child's sense of social exclusion;
- If an educational strategy focuses only on the child's abnormal, distressing behavior, it will fail to take advantage of the creative, competitive, and dynamic energy that often accompanies ADHD;
- The best approach may be to treat this syndrome is to train teachers to manage such children in normal classrooms.
Other treatments attention deficit hyperactivity disorder
- Dietary approach. Certain diets have been suggested for people with ADHD. Several well-conducted studies do not support the effects of dietary sugar and dietary supplements, suggesting that they negatively affect the behavior of those with ADHD, except perhaps in a very small percentage of children. However, various studies have shown improvements in behavior from diets that limit potential allergens (eg, citrus fruits) in the diet. Parents may want to talk to their doctor about eliminating a food-specific diet.
Possible stimuli that influence behavior change include:
Any artificial colors (especially yellow, red or green);
- other chemical additives;
- milk;
- chocolate;
- eggs;
- wheat;
- food products containing salicylates, including all berries, ground red peppers, apples and cider, cloves, grapes, oranges, peaches, peppers, plums, prunes, tomatoes;
- essential fatty acids. Omega-3 fatty acids, which are found in fatty fish and some vegetable oils, are important for normal brain function and may provide some benefits for people with ADHD. It has not yet been determined whether supplementation with polyunsaturated fatty acid compounds such as docosahexaenoic acid and eicosapentaenoic acid provides benefits;
- zinc. Zinc is an important metabolic neurotransmitter that plays a role in ADHD. Its deficiency may in some cases be associated with ADHD. Long-term use of zinc, however, can lead to anemia and other side effects in people without deficiencies, and in these patients it has no effect on ADHD. In any case, testing for micronutrients such as zinc is not routine when evaluating children with suspected ADHD;
- sugar. Although parents often believe that sugar is harmful to children, because... it causes them to become impulsive or hyperactive—research does not confirm this.
- Alternative methods. A number of alternative approaches help children and adults with mild ADHD symptoms. For example, daily massage may help some people with ADHD feel happier, less agitated, less hyperactive, and more focused on tasks. Other alternative approaches that may be helpful include relaxation training and music therapy. These treatments may be useful for symptomatic treatment, but they have not been shown to provide benefit to the underlying disorder.
- Herbs and supplements. Many parents resort to alternative remedies - psychostimulants and other medications. These products include: St. John's wort, ginseng, melatonin, pine bark extract, etc. However, there is no scientific evidence that they are effective.
